Notes from Boehringer Ingelheim webinar 04 September 2012
Andy Durham - Current thoughts of where we are with PPID diagnostics
Andy Durham - Current thoughts of where we are with PPID diagnostics
NOTES MADE DURING WEBINAR - NO RESPONSIBILITY WHATSOEVER IS TAKEN FOR THE ACCURACY OF THESE NOTES
Diagnostic tests for PPID
99% of tests for PPID (at Liphook) now basal plasma ACTH concentration.
Not difficult - collect one sample into EDTA, chill within 3 hrs, centrifuge ASAP, chill during shipping, observe seasonal reference intervals.
Can be used year round and probably better in the autumn.
False positives are rare but likely missing some early cases.
ODST not being used much now - normal horse will suppress cortisol below 27 nmol/L or 1µg/dL 19 hours after 40 µg/kg BW dexamethasone administration. Can’t use in autumn because no seasonal reference ranges. Worry about laminitis risk.
PPID is different in every horse
PPID is a heterogeneous disease (different in every horse) - develops over months if not years - early and late stage cases.
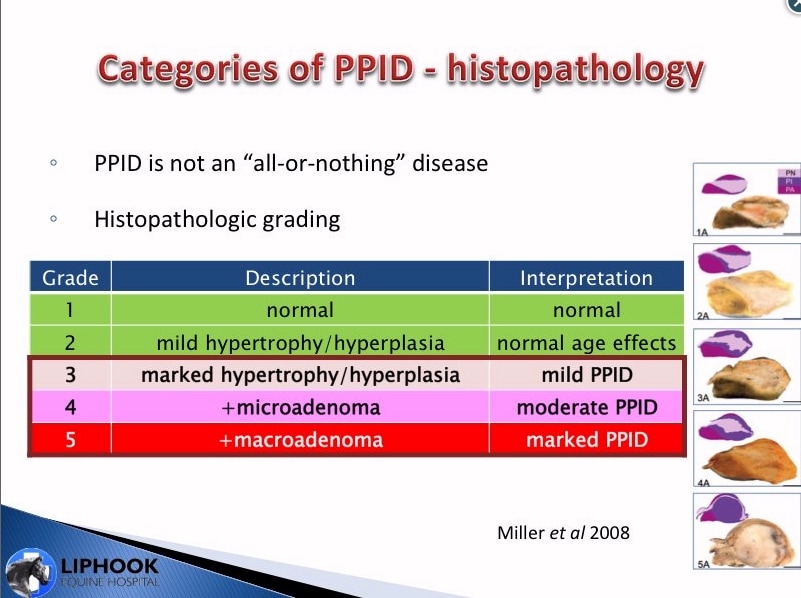
Miller et al. 2008 graded pars intermedias by histology into 5 grades – grades 3 (marked hypertrophy/hyperplasia), 4 (plus microadenoma) and 5 (plus macroadenoma) indicating there are at least 3 stages of PPID.
Diagnostic tests for PPID
99% of tests for PPID (at Liphook) now basal plasma ACTH concentration.
Not difficult - collect one sample into EDTA, chill within 3 hrs, centrifuge ASAP, chill during shipping, observe seasonal reference intervals.
Can be used year round and probably better in the autumn.
False positives are rare but likely missing some early cases.
ODST not being used much now - normal horse will suppress cortisol below 27 nmol/L or 1µg/dL 19 hours after 40 µg/kg BW dexamethasone administration. Can’t use in autumn because no seasonal reference ranges. Worry about laminitis risk.
PPID is different in every horse
PPID is a heterogeneous disease (different in every horse) - develops over months if not years - early and late stage cases.
Miller et al. 2008 graded pars intermedias by histology into 5 grades – grades 3 (marked hypertrophy/hyperplasia), 4 (plus microadenoma) and 5 (plus macroadenoma) indicating there are at least 3 stages of PPID.
Changes in the PI precede clinical signs and abnormal lab results
Dianne McFarlane (ACVIM 2012) examined 120 horses before and after death, 48 normal and 72 PPID according to post mortem histology.
Of the horses with grade 3 PIs (hypertrophy/hyperplasia), only 2/34 (6%)had clinical signs of PPID;
of the horses with grade 4 PIs (microadenomas), only 3/27 (11%) had clinical signs;
many grade 3 and 4 horses had negative ACTH and DST results, the mean ACTH and DST results for grade 3 and grade 4 horses were normal.
The normal horses (grades 1 and 2) all had negative blood results.
All the horses with grade 5 (macroadenomas) PIs had abnormal ACTH and ODSTs, and all but one had clinical signs.
This suggests we are likely to be missing a lot of early PPID cases - 79% of horses with histopathology of PPID had no clinical signs of PPID. Early detection and treatment may help to slow neurodegeneration.
NB RIA was used for ACTH testing, 58 pg/ml cut-off is equivalent to 29 pg/ml with CIA (as used by Liphook) - RIA has higher results than CIA.
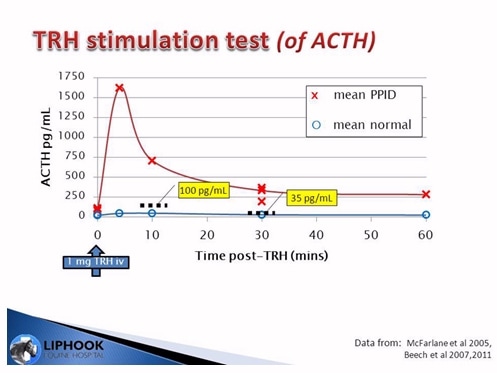
TRH stimulation test
The TRH stimulation test (testing ACTH) currently appears to be the best test for “grey-area” cases (TRH testing cortisol is now largely discredited).
Horses are injected with 1 mg TRH IV, normal horses show very little response to TRH, PPID horses have big surge in ACTH production in response to TRH. Research suggests ACTH tested 10 minutes post TRH uses 100 pg/ml cut-off (30 minutes post TRH uses 35 pg/ml cut-off). Currently no seasonally adjusted reference ranges for TRH stimulation of ACTH.
Dianne McFarlane (ACVIM 2012) examined 120 horses before and after death, 48 normal and 72 PPID according to post mortem histology.
Of the horses with grade 3 PIs (hypertrophy/hyperplasia), only 2/34 (6%)had clinical signs of PPID;
of the horses with grade 4 PIs (microadenomas), only 3/27 (11%) had clinical signs;
many grade 3 and 4 horses had negative ACTH and DST results, the mean ACTH and DST results for grade 3 and grade 4 horses were normal.
The normal horses (grades 1 and 2) all had negative blood results.
All the horses with grade 5 (macroadenomas) PIs had abnormal ACTH and ODSTs, and all but one had clinical signs.
This suggests we are likely to be missing a lot of early PPID cases - 79% of horses with histopathology of PPID had no clinical signs of PPID. Early detection and treatment may help to slow neurodegeneration.
NB RIA was used for ACTH testing, 58 pg/ml cut-off is equivalent to 29 pg/ml with CIA (as used by Liphook) - RIA has higher results than CIA.
TRH stimulation test
The TRH stimulation test (testing ACTH) currently appears to be the best test for “grey-area” cases (TRH testing cortisol is now largely discredited).
Horses are injected with 1 mg TRH IV, normal horses show very little response to TRH, PPID horses have big surge in ACTH production in response to TRH. Research suggests ACTH tested 10 minutes post TRH uses 100 pg/ml cut-off (30 minutes post TRH uses 35 pg/ml cut-off). Currently no seasonally adjusted reference ranges for TRH stimulation of ACTH.
Using CIA (cut-off 29 pg/ml outside of autumn), results under 20 pg/ml are likely to be negative for PPID, results over 40 pg/ml are likely to be positive, results between 20 – 40 pg/ml fall into a “grey area” – these may be early PPID cases.
Testing ACTH 10 minutes post TRH, Liphook found that TRH results generally confirmed negative basal ACTH (<20 pg/ml) and positive basal ACTH (>40 pg/ml). For basal ACTH results between 20 and 40 pg/ml, around 50% of TRH results were positive and 50% negative.
NB "grey-zone" now identified for resting ACTH - 20-40 pg/ml if using CIA with 29 pg/ml cut-off outside of autumn. Generally "grey zone" suggested as cut-off +/- 10 pg/ml.
Treatment and Monitoring
Dose of pergolide
No consensus as to the “correct” dose of pergolide - a horse with mild hyperplasia may respond well to 2 mcg/kg (1 mg/500 kg horse), whereas a horse with a macroadenoma may need a much higher dose. PPID is different in every horse, plus there may be differences in absorption of pergolide between individual horses. Lab tests can be used to monitor response to treatment, but clinical signs must be taken into account as well.
NB interesting to note that Orth et al. 1982 used 10 µg/kg pergolide and this dose was considered safe.
Response to treatment with pergolide
Liphook measured the response to (0.5 – 1 mg) pergolide in over 600 horses.
Follow up tests after 4 – 12 weeks pergolide treatment showed ACTH decreased in 91.8% of horses. 37% had normal ACTH, 38% had a > 50% reduction in ACTH with ACTH remaining above normal, and 25% had a < 50% reduction in ACTH with ACTH remaining above normal. When some of these horses were tested after 6+ months, the response was poorer and 42% had ACTH that had decreased by < 50% from the pre-treatment ACTH. Reasons put forward for this: disease progression (most likely - disease initially controlled and then over time becomes less controlled? (was seasonal rise taken into account?)), increasing tolerance to pergolide, selection bias (poor responders more likely to be retested).
How quickly do horses respond to pergolide?
Liphook found that of 33/39 horses that showed a good or partial response to pergolide, the majority (average 63%) responded within 1 week of starting treatment, an average of 80% showed a response within 2 weeks, and all but one horse (average 91%) had responded within 4 weeks of starting treatment.
When should follow-up testing be carried out?
Follow up testing is recommended 4 weeks after starting pergolide and the dosage should be increased if the response is disappointing.
Regular monitoring of ACTH is recommended, ideally every 3 to 6 months with one test between August and October to see whether PPID is controlled through the seasonal rise.
What about horses that don’t respond to pergolide?
Most horses that do not respond to an initial (2 mcg/kg) dose of pergolide do tend to respond to an increased dose. Some horses may respond in the long-term:
Hal Schott reported at ACVIM 2012 that of 8 PPID horses that had not responded to 2 mcg/kg pergolide at 3 months and 4 mcg/kg at 6 months, but continued to receive 4 mcg/kg, 5 had responded 2 years later, and 6 had responded 3 years later - appears there is potential for horses to respond to pergolide in the longer-term.
Some cases respond when 0.25 mg/kg/12 hrs cyproheptadine is added to a high (10 µg/kg?) dose of pergolide.
Conclusions
Diagnostics
ACTH is preferred to ODST for routine diagnosis.
Early PPID cases are being missed – we can diagnose full-blown PPID with macroadenomas but early cases are not showing characteristic clinical signs or lab tests outside of normal ranges.
TRH stimulation test (of ACTH) might detect cases earlier, could be used following “grey-area” resting ACTH results (20 – 40 pg/ml CIA), but we don’t yet have seasonal references ranges.
Better PPID tests are needed – Liphook are investigating.
Monitoring
Recheck ACTH after a month and adjust dosage of pergolide as required.
Maximum dose is probably 10 µg/kg BW - happy this is safe.
Horses that don’t respond to the maximum dose (10 µg/kg) could either carry on with an affordable dose in the hope that they will eventually respond, or try adding cyproheptadine (0.25 mg/kg every 12 hrs) to the pergolide.
When horses are stable and the PPID appears controlled, it may be possible to reduce the dose – retest to monitor.
This webinar was presented by bi-academy on 04 September 2012 (login required):
http://live.webcasts.unique-media.tv/bil019/interface
Testing ACTH 10 minutes post TRH, Liphook found that TRH results generally confirmed negative basal ACTH (<20 pg/ml) and positive basal ACTH (>40 pg/ml). For basal ACTH results between 20 and 40 pg/ml, around 50% of TRH results were positive and 50% negative.
NB "grey-zone" now identified for resting ACTH - 20-40 pg/ml if using CIA with 29 pg/ml cut-off outside of autumn. Generally "grey zone" suggested as cut-off +/- 10 pg/ml.
Treatment and Monitoring
Dose of pergolide
No consensus as to the “correct” dose of pergolide - a horse with mild hyperplasia may respond well to 2 mcg/kg (1 mg/500 kg horse), whereas a horse with a macroadenoma may need a much higher dose. PPID is different in every horse, plus there may be differences in absorption of pergolide between individual horses. Lab tests can be used to monitor response to treatment, but clinical signs must be taken into account as well.
NB interesting to note that Orth et al. 1982 used 10 µg/kg pergolide and this dose was considered safe.
Response to treatment with pergolide
Liphook measured the response to (0.5 – 1 mg) pergolide in over 600 horses.
Follow up tests after 4 – 12 weeks pergolide treatment showed ACTH decreased in 91.8% of horses. 37% had normal ACTH, 38% had a > 50% reduction in ACTH with ACTH remaining above normal, and 25% had a < 50% reduction in ACTH with ACTH remaining above normal. When some of these horses were tested after 6+ months, the response was poorer and 42% had ACTH that had decreased by < 50% from the pre-treatment ACTH. Reasons put forward for this: disease progression (most likely - disease initially controlled and then over time becomes less controlled? (was seasonal rise taken into account?)), increasing tolerance to pergolide, selection bias (poor responders more likely to be retested).
How quickly do horses respond to pergolide?
Liphook found that of 33/39 horses that showed a good or partial response to pergolide, the majority (average 63%) responded within 1 week of starting treatment, an average of 80% showed a response within 2 weeks, and all but one horse (average 91%) had responded within 4 weeks of starting treatment.
When should follow-up testing be carried out?
Follow up testing is recommended 4 weeks after starting pergolide and the dosage should be increased if the response is disappointing.
Regular monitoring of ACTH is recommended, ideally every 3 to 6 months with one test between August and October to see whether PPID is controlled through the seasonal rise.
What about horses that don’t respond to pergolide?
Most horses that do not respond to an initial (2 mcg/kg) dose of pergolide do tend to respond to an increased dose. Some horses may respond in the long-term:
Hal Schott reported at ACVIM 2012 that of 8 PPID horses that had not responded to 2 mcg/kg pergolide at 3 months and 4 mcg/kg at 6 months, but continued to receive 4 mcg/kg, 5 had responded 2 years later, and 6 had responded 3 years later - appears there is potential for horses to respond to pergolide in the longer-term.
Some cases respond when 0.25 mg/kg/12 hrs cyproheptadine is added to a high (10 µg/kg?) dose of pergolide.
Conclusions
Diagnostics
ACTH is preferred to ODST for routine diagnosis.
Early PPID cases are being missed – we can diagnose full-blown PPID with macroadenomas but early cases are not showing characteristic clinical signs or lab tests outside of normal ranges.
TRH stimulation test (of ACTH) might detect cases earlier, could be used following “grey-area” resting ACTH results (20 – 40 pg/ml CIA), but we don’t yet have seasonal references ranges.
Better PPID tests are needed – Liphook are investigating.
Monitoring
Recheck ACTH after a month and adjust dosage of pergolide as required.
Maximum dose is probably 10 µg/kg BW - happy this is safe.
Horses that don’t respond to the maximum dose (10 µg/kg) could either carry on with an affordable dose in the hope that they will eventually respond, or try adding cyproheptadine (0.25 mg/kg every 12 hrs) to the pergolide.
When horses are stable and the PPID appears controlled, it may be possible to reduce the dose – retest to monitor.
This webinar was presented by bi-academy on 04 September 2012 (login required):
http://live.webcasts.unique-media.tv/bil019/interface
Notes from Boehringer Ingelheim webinar 04 September 2012
Andy Durham and Cathy McGowan - questions asked
Q. Likely diagnosis for 17 year old laminitic pony very high cortisol but normal insulin?
Andy: Cortisol has no diagnostic value for PPID. Where cortisol is high, probably related to pain from current laminitis. Normal resting insulin doesn't mean horse isn't insulin resistant and that horse won't experience marked hyperinsulinaemia after eating sugar. Dismiss cortisol result, test ACTH and do glucose challenge.
Q. Laminitic pony high insulin, high cortisol and normal ACTH – could this be adrenal neoplasm?
Andy: Cortisol-producing adrenal neoplasia very rare (van den Kolk had a case) – sounds like EMS not PPID. Cortisol probably reflects pain - ignore. Look at body condition etc.
PPID doesn't usually involve hyperadrenocorticism – there's evidence that the ACTH produced in PPID horses is not very bioactive – can pick it up in lab test but it doesn’t really stimulate adrenal glands in majority of cases. Cortisol further removed from the condition than it might be in other species.
Q. How useful is trilostane?
Cathy: might add trilostane to a pergolide regime if felt laminitis was completely out of control – really just last ditch effort – don’t use routinely. Had good effects against laminitis where stress involved e.g. transport, but not first line remedy.
Q. Danger of treating horses with high ACTH with high levels of pergolide?
Andy: High ACTH (say 1000 pg/ml) doesn’t necessarily mean need high dose of pergolide – often response can be as good if not better than lower ACTH levels. If failure to respond to lower doses, 10 mcg/kg seems fine, nothing more serious than inappetance seen. Dave Rendle found 20 mgc/kg causes reversible neurologic signs - general hyperexcitablility (in non-PPID horses) – nothing more serious. Andy hasn’t come across any suggestions of safety issues – Hal Schott found no serious side effects up to 8 mcg/kg.
Q. Can we be sure pergolide is causing effect of lowering ACTH (rather than ACTH decreasing naturally)?
Andy: We don’t really know, but horses with high ACTH usually have macroadenomas in pituitary glands – not likely to spontaneously reverse or improve naturally – likely constant battering of PI with dopamine agonist if improvement seen. Hypertrophy could potentially come and go a bit, but not macroadenomas.
Q. PU/PD in PPID?
PU/PD not particularly associated with diagnosis in Cathy’s study because horses lived out but it did occur in 3 x as many horses with PPID as normal aged horses. Will miss a lot of cases in horses that live out – it’s the PU that owners pick up when mucking out, rather than PD per se.
Q. Treatment with pergolide in early stages of disease – does it potentially slow progress of disease?
Cathy: We don’t know – Dianne McFarlane and others have shown that hyperplasia progressively gets worse (to adenomas) - theoretically hyperplasia (from pumping out lots of hormones) might be arrested before it goes further – it is a degenerative disease of old age, it is going to continue, but you might buy more time by treating earlier.
Q. PPID horse, once laminitis under control, and stable on treatment, can they return to grass and live a normal life?
Andy: All different, require different monitoring. Some evidence insulin is a better marker for laminitis prediction than ACTH – can have very high ACTH with no laminitis history at all. PPID cases with high insulin (resting or after OGT) are the ones to be more worried about. Check insulin response before returning to grazing – wouldn’t return to grazing if high insulin – can’t generalise. PPID isn’t like EMS where most cases are fat and benefit from coming off grass. Some PPID cases are too thin and need to be careful not to over-restrict – individual tailoring according to body condition, teeth, insulin response.
Cathy: Would base return to pasture on insulin response to glucose challenge - does CGIT (in hospital) rather than OGT – point is what does insulin do to glucose challenge, as that’s what grass is going to do.
Q. Value of insulin to glucose ratio?
Andy: insulin:glucose ratio specifically is not worth time & effort in calculating! Worth a look at glucose as diabetes mellitus cases do crop up – in ideal world look at ACTH, insulin and glucose - but ratio of no great value. Insulin values are key, whether resting insulin or glucose challenge – very important part of assessment of PPID case.
Q. Borderline ACTH and positive TRH – when would you retest with TRH?
Andy: Use TRH stimulation test following borderline resting ACTH. Retest for TRH stimulation probably same timeline as resting ACTH – 1-2 months but no evidence to back this up. No data on using TRH in autumn so currently can’t use – logical to assume TRH response will be greater in the autumn. Dianne McFarlane hoping to do research in Sept this year/next year to see autumnal response to TRH. TRH can be bought from Sigma Aldrich pharmaceutical grade but can’t be bought in UK as medical grade, and only in large quantities, so expensive. Liphook have arranged with VMD to supply it (diluted out and frozen) at around £10 for 1mg dose plus lab fee for ACTH £18.50.
Q. Pergolide treatment in mares in foal?
Cathy: limited experience in pregnant mares – all cases past breeding age. Report from TB stud farm in Australia, comfortable with mares on pergolide but always stopped 1-2 wks before lactation
Andy: PPID horses tend to be older and often difficult to get in foal so very little experience. Issue is lactation suppression. Reports of pregnant mares on pergolide that don’t develop an udder – logical physiologically in terms of dopamine agonism suppressing prolactin, others report mares on pergolide that have gone into a normal lactation. Need to make sure udder is developing towards end of pregnancy, if not perhaps reduce or even stop pergolide.
Q. Any comments on the use of extended day length management for PPID horses in winter?
Cathy: clearly autumn laminitis episodes and peptides increase during autumn period, so in theory potential to decrease peptide increase, but data in Queensland with very little day length variation between summer and winter (2 hrs max) still have as dramatic autumn changes.
Andy: if day length is a factor it can’t be absolute day length, otherwise there would be an issue in the spring as well as autumn when day lengths of similar duration so it must be specifically decreasing day lengths.
Q. Has every horse that is diagnosed with PPID had laminitis?
Cathy: definitely not. PPID doesn’t always present with laminitis – only around 10% of PPID horses had laminitis in Australian research. PPID predisposes to laminitis. Many owners don’t recognise PPID, often laminitis is what makes them notice, best to diagnose PPID before laminitis occurs and prevent it.
Andy: PPID horses don’t all get laminitis, some don’t tend to get laminitis, particularly older horses 30+ tend to have lower insulin, higher ACTH and less laminitis. Plenty of cases never get laminitis. Laminitis is often what gets the vet in.
Q. Any risks of Bute and Pergolide together?
Andy: Not aware of any evidence, and frequently used together so unlikely, had plenty of cases on both drugs with no problems.
(NB TLS is currently investigating the concurrent use of Phenylbutazone (Bute) (and other NSAIDs e.g. Danilon) and Pergolide.
Prascend is approx. 90% bound to plasma proteins.
Phenylbutazone is >98% bound to plasma proteins.
Suxibizone (Danilon) is highly bound to plasma proteins.
The datasheets for all of these drugs advise caution when using concurrently with other highly plasma protein bound drugs.)
Andy Durham and Cathy McGowan - questions asked
Q. Likely diagnosis for 17 year old laminitic pony very high cortisol but normal insulin?
Andy: Cortisol has no diagnostic value for PPID. Where cortisol is high, probably related to pain from current laminitis. Normal resting insulin doesn't mean horse isn't insulin resistant and that horse won't experience marked hyperinsulinaemia after eating sugar. Dismiss cortisol result, test ACTH and do glucose challenge.
Q. Laminitic pony high insulin, high cortisol and normal ACTH – could this be adrenal neoplasm?
Andy: Cortisol-producing adrenal neoplasia very rare (van den Kolk had a case) – sounds like EMS not PPID. Cortisol probably reflects pain - ignore. Look at body condition etc.
PPID doesn't usually involve hyperadrenocorticism – there's evidence that the ACTH produced in PPID horses is not very bioactive – can pick it up in lab test but it doesn’t really stimulate adrenal glands in majority of cases. Cortisol further removed from the condition than it might be in other species.
Q. How useful is trilostane?
Cathy: might add trilostane to a pergolide regime if felt laminitis was completely out of control – really just last ditch effort – don’t use routinely. Had good effects against laminitis where stress involved e.g. transport, but not first line remedy.
Q. Danger of treating horses with high ACTH with high levels of pergolide?
Andy: High ACTH (say 1000 pg/ml) doesn’t necessarily mean need high dose of pergolide – often response can be as good if not better than lower ACTH levels. If failure to respond to lower doses, 10 mcg/kg seems fine, nothing more serious than inappetance seen. Dave Rendle found 20 mgc/kg causes reversible neurologic signs - general hyperexcitablility (in non-PPID horses) – nothing more serious. Andy hasn’t come across any suggestions of safety issues – Hal Schott found no serious side effects up to 8 mcg/kg.
Q. Can we be sure pergolide is causing effect of lowering ACTH (rather than ACTH decreasing naturally)?
Andy: We don’t really know, but horses with high ACTH usually have macroadenomas in pituitary glands – not likely to spontaneously reverse or improve naturally – likely constant battering of PI with dopamine agonist if improvement seen. Hypertrophy could potentially come and go a bit, but not macroadenomas.
Q. PU/PD in PPID?
PU/PD not particularly associated with diagnosis in Cathy’s study because horses lived out but it did occur in 3 x as many horses with PPID as normal aged horses. Will miss a lot of cases in horses that live out – it’s the PU that owners pick up when mucking out, rather than PD per se.
Q. Treatment with pergolide in early stages of disease – does it potentially slow progress of disease?
Cathy: We don’t know – Dianne McFarlane and others have shown that hyperplasia progressively gets worse (to adenomas) - theoretically hyperplasia (from pumping out lots of hormones) might be arrested before it goes further – it is a degenerative disease of old age, it is going to continue, but you might buy more time by treating earlier.
Q. PPID horse, once laminitis under control, and stable on treatment, can they return to grass and live a normal life?
Andy: All different, require different monitoring. Some evidence insulin is a better marker for laminitis prediction than ACTH – can have very high ACTH with no laminitis history at all. PPID cases with high insulin (resting or after OGT) are the ones to be more worried about. Check insulin response before returning to grazing – wouldn’t return to grazing if high insulin – can’t generalise. PPID isn’t like EMS where most cases are fat and benefit from coming off grass. Some PPID cases are too thin and need to be careful not to over-restrict – individual tailoring according to body condition, teeth, insulin response.
Cathy: Would base return to pasture on insulin response to glucose challenge - does CGIT (in hospital) rather than OGT – point is what does insulin do to glucose challenge, as that’s what grass is going to do.
Q. Value of insulin to glucose ratio?
Andy: insulin:glucose ratio specifically is not worth time & effort in calculating! Worth a look at glucose as diabetes mellitus cases do crop up – in ideal world look at ACTH, insulin and glucose - but ratio of no great value. Insulin values are key, whether resting insulin or glucose challenge – very important part of assessment of PPID case.
Q. Borderline ACTH and positive TRH – when would you retest with TRH?
Andy: Use TRH stimulation test following borderline resting ACTH. Retest for TRH stimulation probably same timeline as resting ACTH – 1-2 months but no evidence to back this up. No data on using TRH in autumn so currently can’t use – logical to assume TRH response will be greater in the autumn. Dianne McFarlane hoping to do research in Sept this year/next year to see autumnal response to TRH. TRH can be bought from Sigma Aldrich pharmaceutical grade but can’t be bought in UK as medical grade, and only in large quantities, so expensive. Liphook have arranged with VMD to supply it (diluted out and frozen) at around £10 for 1mg dose plus lab fee for ACTH £18.50.
Q. Pergolide treatment in mares in foal?
Cathy: limited experience in pregnant mares – all cases past breeding age. Report from TB stud farm in Australia, comfortable with mares on pergolide but always stopped 1-2 wks before lactation
Andy: PPID horses tend to be older and often difficult to get in foal so very little experience. Issue is lactation suppression. Reports of pregnant mares on pergolide that don’t develop an udder – logical physiologically in terms of dopamine agonism suppressing prolactin, others report mares on pergolide that have gone into a normal lactation. Need to make sure udder is developing towards end of pregnancy, if not perhaps reduce or even stop pergolide.
Q. Any comments on the use of extended day length management for PPID horses in winter?
Cathy: clearly autumn laminitis episodes and peptides increase during autumn period, so in theory potential to decrease peptide increase, but data in Queensland with very little day length variation between summer and winter (2 hrs max) still have as dramatic autumn changes.
Andy: if day length is a factor it can’t be absolute day length, otherwise there would be an issue in the spring as well as autumn when day lengths of similar duration so it must be specifically decreasing day lengths.
Q. Has every horse that is diagnosed with PPID had laminitis?
Cathy: definitely not. PPID doesn’t always present with laminitis – only around 10% of PPID horses had laminitis in Australian research. PPID predisposes to laminitis. Many owners don’t recognise PPID, often laminitis is what makes them notice, best to diagnose PPID before laminitis occurs and prevent it.
Andy: PPID horses don’t all get laminitis, some don’t tend to get laminitis, particularly older horses 30+ tend to have lower insulin, higher ACTH and less laminitis. Plenty of cases never get laminitis. Laminitis is often what gets the vet in.
Q. Any risks of Bute and Pergolide together?
Andy: Not aware of any evidence, and frequently used together so unlikely, had plenty of cases on both drugs with no problems.
(NB TLS is currently investigating the concurrent use of Phenylbutazone (Bute) (and other NSAIDs e.g. Danilon) and Pergolide.
Prascend is approx. 90% bound to plasma proteins.
Phenylbutazone is >98% bound to plasma proteins.
Suxibizone (Danilon) is highly bound to plasma proteins.
The datasheets for all of these drugs advise caution when using concurrently with other highly plasma protein bound drugs.)

 RSS Feed
RSS Feed