In particular:
- important to recognise early and advanced PPID symptoms, early signs are often subtle and variable and include late shedding of winter coat, patchy longer/lighter coloured hairs, regional fat deposits, loss of topline, easy keeper becomes hard to keep weight on, depression & lethargy, footsoreness and chronic laminitis.
More advanced signs include "woolly mammoth" hair coat, recurrent infections e.g. hoof and tooth abscesses & sinusitis, excess drinking/urination, abnormal sweating.
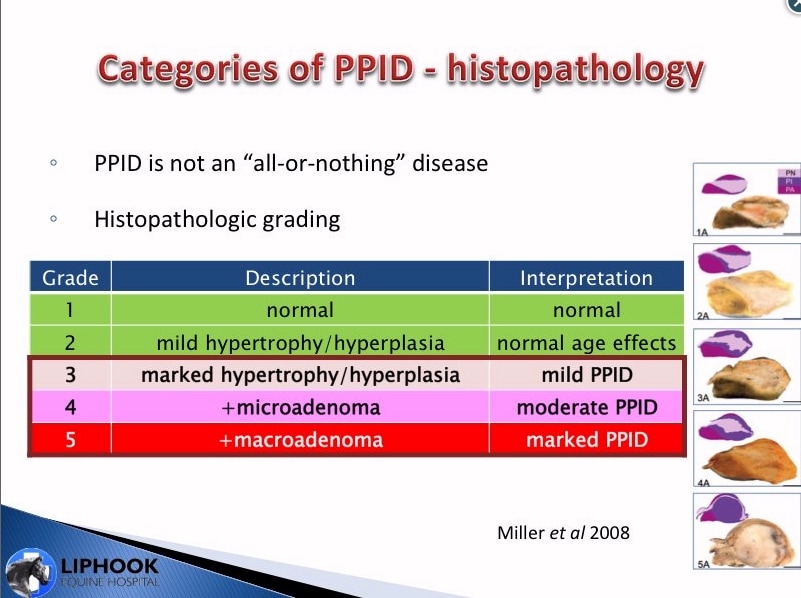
- Miller graded pituitary glands into 1 and 2 = normal, 3 = mild PPID, 4 = moderate PPID and 5 = advanced PPID. Diagnostic blood tests only picked up grade 5 and some grade 4 cases of PPID, but mild and moderate PPID cases are generally not detected by current testing. If a horse has clinical signs but negative test results, keep testing as eventually a positive result is likely.
- Horses that are obese and have EMS are predisposed to PPID.
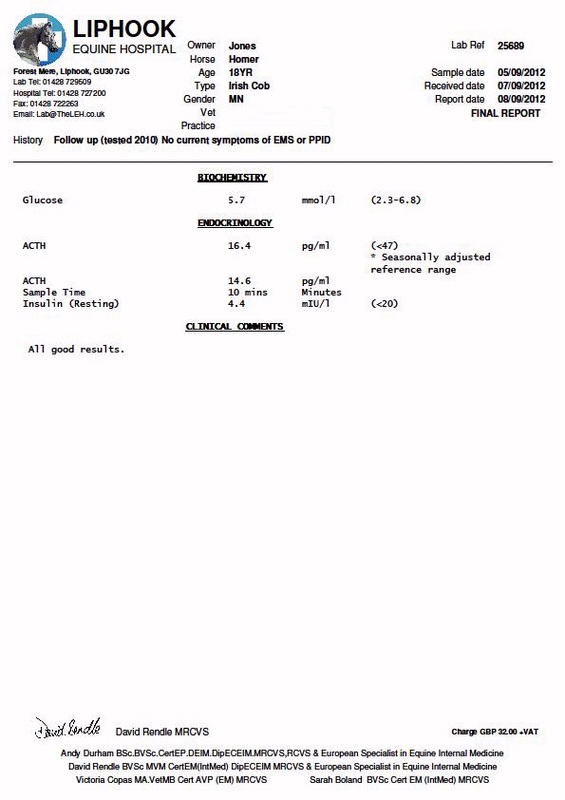
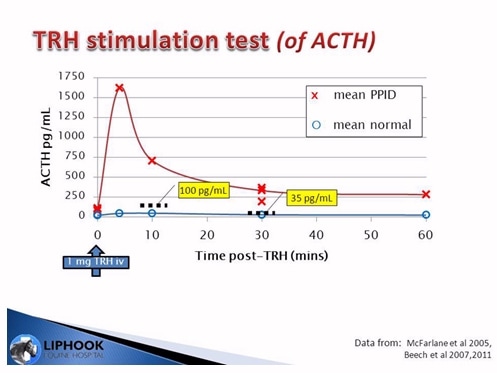
- ACTH is the easiest screening test and autumn is the best time to test using seasonal reference ranges for ACTH. TRH stimulation test (of ACTH) may be a more sensitive test for diagnosing early PPID cases.
- Horses may need increased pergolide during the autumn seasonal rise - test ACTH to check control of PPID. Even when diagnosis is obvious from clinical signs, testing ACTH gives a measure of severity and response to treatment.
- caring for the PPID horse includes giving pergolide, checking insulin levels, good nutrition (vitamin E and anti-oxidants), hoof care, clipping, deworming, regular dental checks, exercise if possible.
- not all horses with PPID are insulin resistant - insulin should be tested (basal insulin and glucose and/or oral sugar test) to make informed decisions about nutrition, e.g. able to graze or not. Not all horses with PPID will get laminitis - laminitis is connected to insulin resistance. If not insulin resistant, many older horses do better on grass.
- every case of PPID is different and must be managed individually.
Listen to the archived recording at www.thehorse.com
Read notes of the session




 RSS Feed
RSS Feed