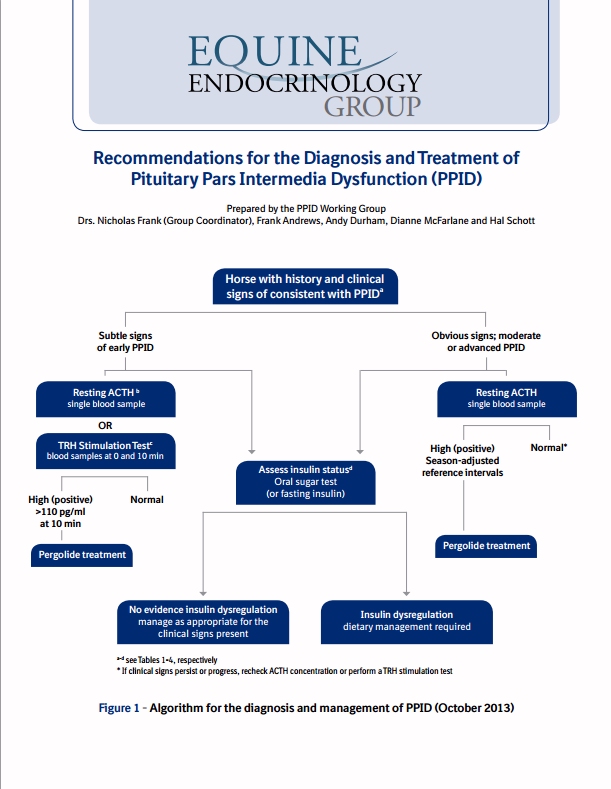
| The Equine Endocrinology Group has released updated Recommendations for the Diagnosis and Treatment of PPID: Horses with subtle signs of PPID are recommended to have a resting ACTH or TRH stimulation of ACTH test carried out (TLS recommends having a resting ACTH test carried out initially). Horses with obvious signs of PPID should have a resting ACTH test carried out. Although a single blood sample is suggested for the resting ACTH test, it is pointed out that resting ACTH concentrations are variable, so another sample should be submitted (or the TRH stimulation test carried out) when results are equivocal. Early PPID cases may not be picked up by the resting ACTH test - retesting between August and October (during the seasonal rise) or performing a TRH stimulation test between December and June is recommended in these cases. |
As in the earlier guidelines, clinical symptoms of PPID are given split into early: decreased athletic performance, change in attitude/lethargy, delayed haircoat shedding, regional hairiness (hypertrichosis), change in body shape, regional adiposity (fat pads), laminitis;
and advanced: lethargy, all over hairiness (hypertrichosis), failure to shed haircoat, muscle loss, pot belly, abnormal sweating (increased or decreased), increased drinking/urination, recurrent infections, regional adiposity, loss of seasons/infertility, laminitis, raised glucose levels (hyperglycaemia), neurological symptoms/blindness.
Instructions are given for preparing the blood samples for ACTH testing, and the warning included that freezing samples without prior centrifugation can cause falsely high results.
Interestingly, Liphook's cut-offs for resting ACTH are given as 47 pg/ml Aug-Oct, 29 pg/ml rest of year (using Immulite CIA), and Cornell's (also using CIA?) as 35 pg/ml Nov-July and 100 pg/ml mid Aug-mid Oct, although this is qualified as needing further research. No mention is made of the "grey area" that Andy Durham and David Rendle of Liphook have talked about of 20 - 40 pg/ml Nov-July (and therefore it is assumed approx. 10 pg/ml either side of 47 Aug-Oct), when further testing is recommended - although the Recommendations do suggest further testing for results near the cut-off.
The suggested cut-offs for the TRH stimulation of ACTH have been raised slightly - now 110 pg/ml exactly 10 minutes after TRH administration and 65 pg/ml 30 minutes after TRH administration. The TRH stimulation of ACTH is currently not validated for use between July and November (inclusive), and further research is ongoing to verify the above suggested cut-offs.
As part of the workup for a diagnosis of PPID, it is suggested that insulin status is assessed (and glucose). The EEG now suggests using the oral sugar test (OST) as the first choice for assessing insulin status. However, if the owner is concerned about the OST increasing laminitis risk, a fasting insulin concentration should be measured first and if normal, then the OST should be carried out (this would involve 2 vet visits). Liphook have confirmed that they are happy for owners in the UK to use Karo Light corn syrup, i.e. carry out the OST rather than the in-feed glucose test which uses a much larger amount of glucose - Karo Light corn syrup can be purchased from Amazon in the UK.
Owners worry about fasting their horse overnight for the fasting insulin test - the Recommendations suggest leaving one flake of hay at 10 pm and collecting blood the next morning.
It is pointed out that a normal fasting insulin result is not diagnostically significant - only an above normal insulin result is significant.
A list of potential tests (for PPID) that are not commercially available is given - if only they were available now, but hopefully in the future! They include (as you would expect): Alpha-MSH, bioactive ACTH, POMC, beta-endorphin and CLIP. TLS has been saying for some time that the best test for PPID has to be to measure as many of the affected hormones as possible...
And the list of tests no longer recommended for PPID diagnosis includes anything to do with cortisol!
It is now recommended that pergolide/Prascend is "introduced gradually by giving partial doses for the first four days or by administering half the dose morning and evening." Excellent! NB if you are in the UK, your vet can ask BI for a pill splitter - see Splitting Prascend tablets.
Suggestions are given for the response you might expect to see to treatment with pergolide/Prascend:
Within 30 days - improved attitude, decreased drinking/urination, increased activity and reduced hyperglycaemia.
Anything from 1 to 12 months - improvements in haircoat abnormalities, less of a pot-bellied appearance, fewer infections, improved topline, less laminitis.
Treatment should be continued for at least 2 months before conclusions can be made about changes to symptoms.
Retesting after 30 days of treatment is suggested to assess response to treatment. If test results are normal the dose is not increased. If test results remain above normal but clinical symptoms have improved, the dose can either remain the same or be increased. If test results remain above normal and clinical symptoms have not improved, the dose of pergolide/Prascend should be increased (and possibly the addition of cyproheptadine considered).

 RSS Feed
RSS Feed