| For many horses, barefoot rehabilitation using boots and pads works best, as feet can be fully protected and supported whilst allowing for the short trimming intervals (often 1-2 weekly) that may be needed to keep the feet perfectly aligned following rotation, plus owners can keep the feet clean and healthy, and importantly weight bearing on the less-than-well-connected hoof walls can be reduced. Pete Ramey explains the advantages of using hoof boots and pads following laminitis in his article "Boots and Pads: A True Breakthrough in Healing". Boots and pads can be indispensable from the moment laminitis strikes - some horses are more comfortable with thick pads even when on a deep conforming bed, and keeping a padded boot on the supporting foot whilst the other foot is trimmed or x-rayed can significantly increase the comfort - and willingness - of the horse. Once the feet have been correctly realigned with a derotating trim, boots and pads can be used to protect and support the feet as the horse returns to movement, whether gradually increasing access to a safe turnout area or building up in-hand exercise. TLS director Karen's mare Ziggy had laminitis in winter 2009. Hoof wall grooving and heart bar shoes followed and her feet were fully realigned, but Ziggy never became totally sound, until in 2012 the heart bar shoes were removed for further x-rays and Ziggy walked out sound for the first time in years. She has remained barefoot ever since, fitted with boots and pads and has never looked back. The Boot Bank will enable owners of horses recovering from laminitis to borrow boots short-term, perhaps because they want to try boots before they buy their own, or because with money being spent on blood tests and x-rays, they may not be able to afford to buy new boots as soon as their horse needs them, or because they may not be sure of the size they need, or their horse's feet may have changed shape during rehab - borrowing means they can always use the correct size TLS hopes that by loaning boots to owners, laminitic horses will get the support and comfort that they need and be able to return to movement as soon as it is safe to do so, thereby speeding up their recovery. TLS is dependent on donations and is appealing for old but usable boots of all makes and sizes ready for the next laminitic horse or pony that needs help. If you have boots that you would be willing to donate, please email us at [email protected]. | |
|
The Laminitis Site is appealing for donations of new or used hoof boots for the Boot Bank it is setting up.
3 Comments
The dexamethasone suppression test is no longer suggested - hurray!
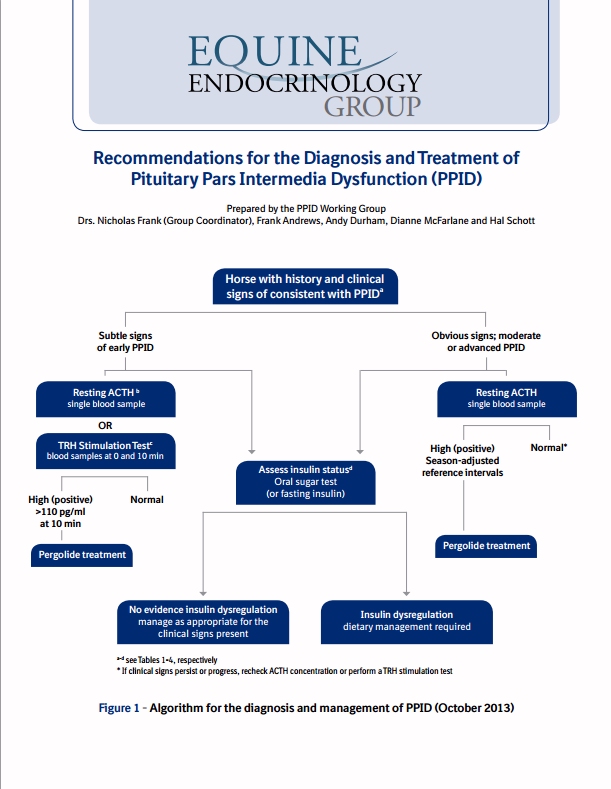
As in the earlier guidelines, clinical symptoms of PPID are given split into early: decreased athletic performance, change in attitude/lethargy, delayed haircoat shedding, regional hairiness (hypertrichosis), change in body shape, regional adiposity (fat pads), laminitis; and advanced: lethargy, all over hairiness (hypertrichosis), failure to shed haircoat, muscle loss, pot belly, abnormal sweating (increased or decreased), increased drinking/urination, recurrent infections, regional adiposity, loss of seasons/infertility, laminitis, raised glucose levels (hyperglycaemia), neurological symptoms/blindness. Instructions are given for preparing the blood samples for ACTH testing, and the warning included that freezing samples without prior centrifugation can cause falsely high results. Interestingly, Liphook's cut-offs for resting ACTH are given as 47 pg/ml Aug-Oct, 29 pg/ml rest of year (using Immulite CIA), and Cornell's (also using CIA?) as 35 pg/ml Nov-July and 100 pg/ml mid Aug-mid Oct, although this is qualified as needing further research. No mention is made of the "grey area" that Andy Durham and David Rendle of Liphook have talked about of 20 - 40 pg/ml Nov-July (and therefore it is assumed approx. 10 pg/ml either side of 47 Aug-Oct), when further testing is recommended - although the Recommendations do suggest further testing for results near the cut-off. The suggested cut-offs for the TRH stimulation of ACTH have been raised slightly - now 110 pg/ml exactly 10 minutes after TRH administration and 65 pg/ml 30 minutes after TRH administration. The TRH stimulation of ACTH is currently not validated for use between July and November (inclusive), and further research is ongoing to verify the above suggested cut-offs. As part of the workup for a diagnosis of PPID, it is suggested that insulin status is assessed (and glucose). The EEG now suggests using the oral sugar test (OST) as the first choice for assessing insulin status. However, if the owner is concerned about the OST increasing laminitis risk, a fasting insulin concentration should be measured first and if normal, then the OST should be carried out (this would involve 2 vet visits). Liphook have confirmed that they are happy for owners in the UK to use Karo Light corn syrup, i.e. carry out the OST rather than the in-feed glucose test which uses a much larger amount of glucose - Karo Light corn syrup can be purchased from Amazon in the UK. Owners worry about fasting their horse overnight for the fasting insulin test - the Recommendations suggest leaving one flake of hay at 10 pm and collecting blood the next morning. It is pointed out that a normal fasting insulin result is not diagnostically significant - only an above normal insulin result is significant. A list of potential tests (for PPID) that are not commercially available is given - if only they were available now, but hopefully in the future! They include (as you would expect): Alpha-MSH, bioactive ACTH, POMC, beta-endorphin and CLIP. TLS has been saying for some time that the best test for PPID has to be to measure as many of the affected hormones as possible... And the list of tests no longer recommended for PPID diagnosis includes anything to do with cortisol! It is now recommended that pergolide/Prascend is "introduced gradually by giving partial doses for the first four days or by administering half the dose morning and evening." Excellent! NB if you are in the UK, your vet can ask BI for a pill splitter - see Splitting Prascend tablets. Suggestions are given for the response you might expect to see to treatment with pergolide/Prascend: Within 30 days - improved attitude, decreased drinking/urination, increased activity and reduced hyperglycaemia. Anything from 1 to 12 months - improvements in haircoat abnormalities, less of a pot-bellied appearance, fewer infections, improved topline, less laminitis. Treatment should be continued for at least 2 months before conclusions can be made about changes to symptoms. Retesting after 30 days of treatment is suggested to assess response to treatment. If test results are normal the dose is not increased. If test results remain above normal but clinical symptoms have improved, the dose can either remain the same or be increased. If test results remain above normal and clinical symptoms have not improved, the dose of pergolide/Prascend should be increased (and possibly the addition of cyproheptadine considered). |
News
What's new in research New Dengie Laminitis Brochure uses TLS photos WHW new laminitis leaflet2020 Global Equine Endocrine Symposium proceedings Articles about feet December 2019 Autumn Laminitis with Danica Pollard Free ACTH Testing Do all IR/EMS horses have laminitis? Clinical signs of PPID may vary with location Velagliflozin - preventative treatment for endocrinopathic laminitis? USEF allows pergolide to be taken by competing horses Pergolide molasses-flavoured paste available in UK NEHS 2018 Risk factors for EMS/Endocrinopathic Laminitis Seasonal rise in pituitary hormonesPPID - weekly ACTH cutoffs now being used Sole Support Do you CARE about laminitis? Pituitary Pars Intermedia Dysfunction - The Arabian Magazine EMS & Insulin Dysregulation - The Arabian Magazine Laminitis and the Feet - The Arabian Magazine The Arabian Magazine Laminitis article Paddock Paradise in French New EEG Recommendations for the diagnosis and treatment of PPID Archives
February 2024
Categories |




 RSS Feed
RSS Feed