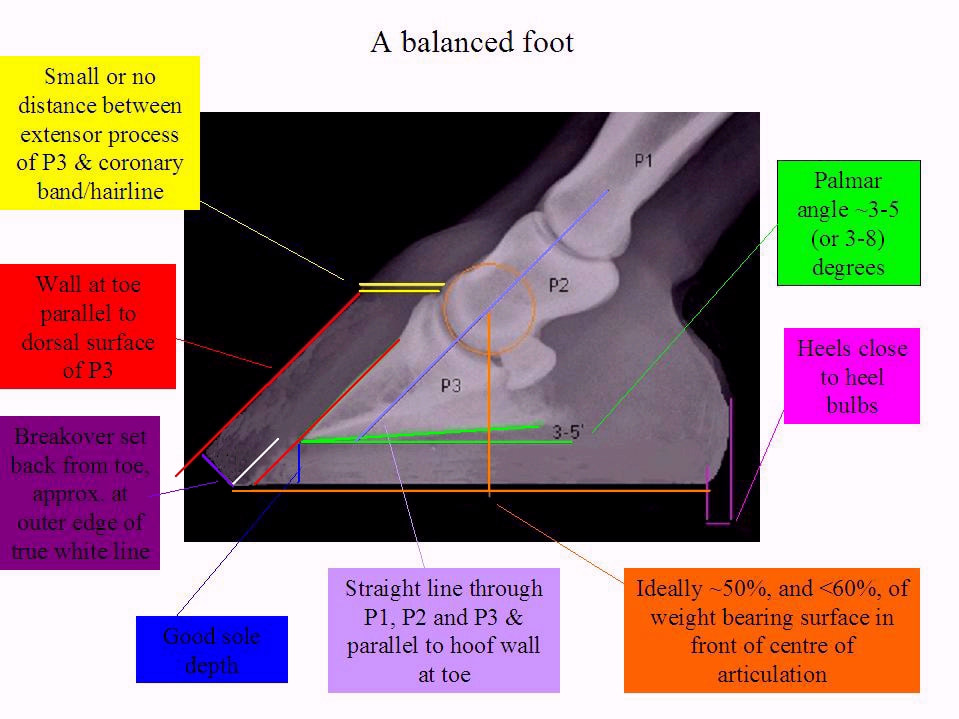
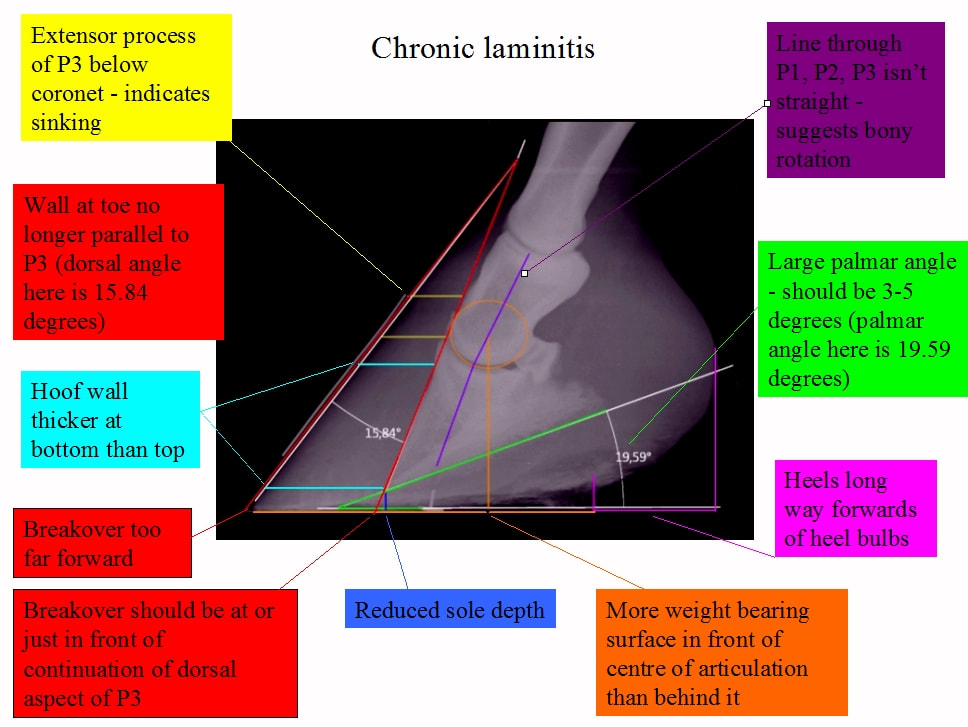
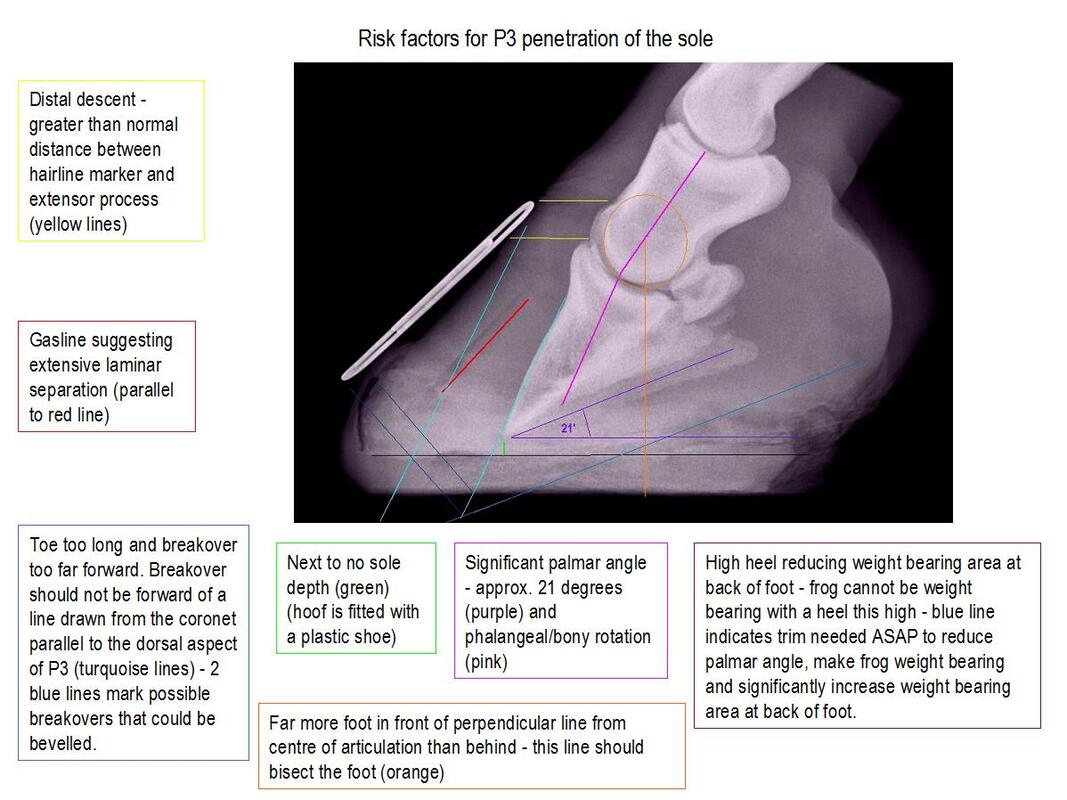
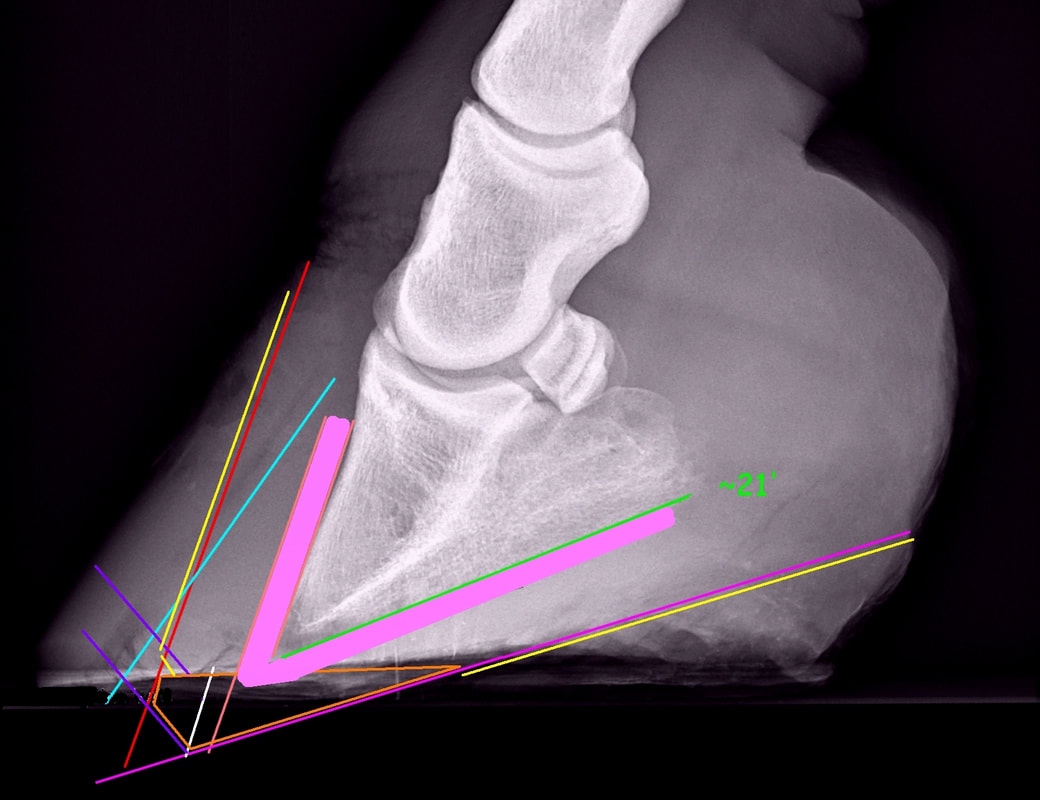
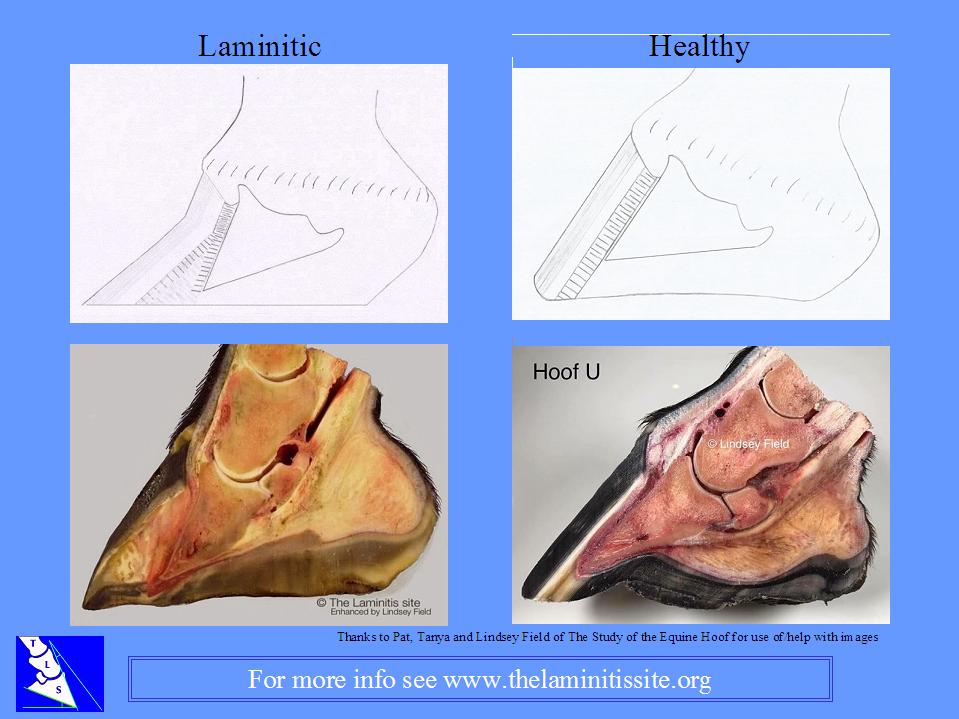
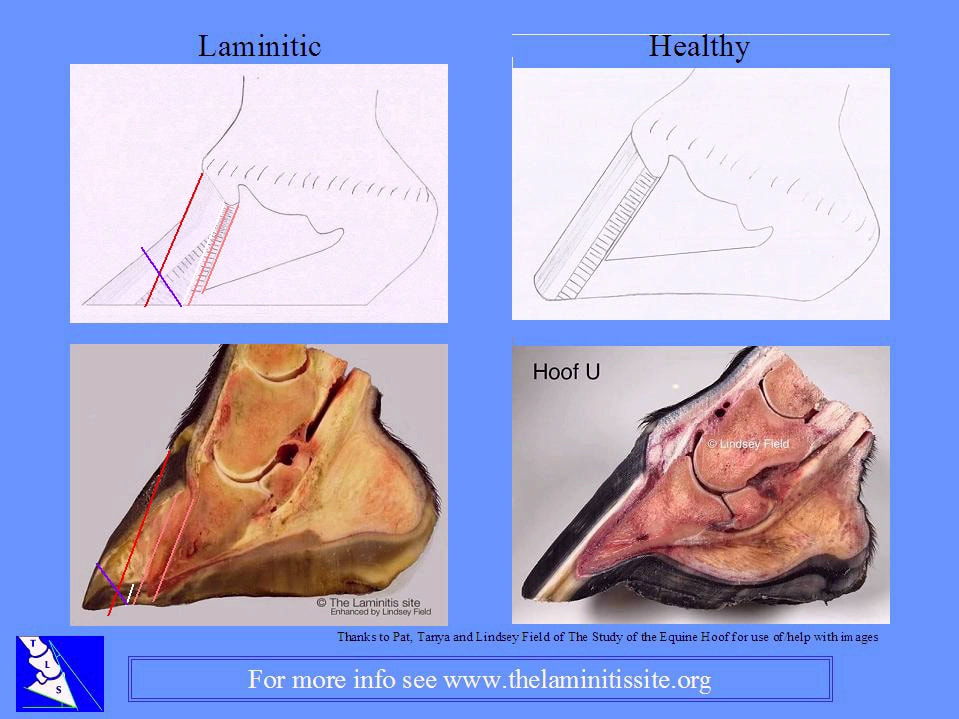
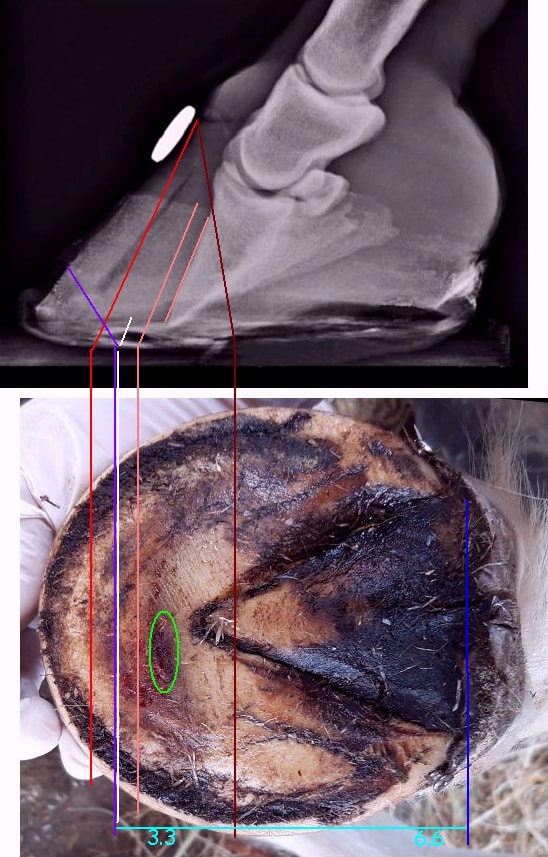
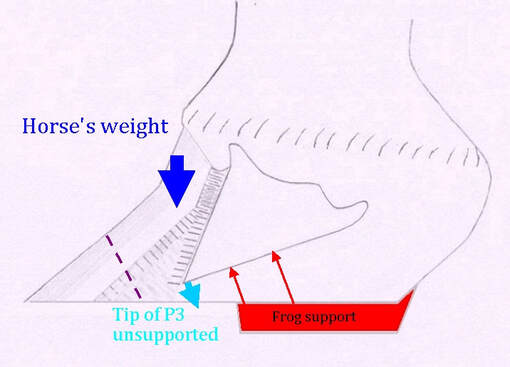
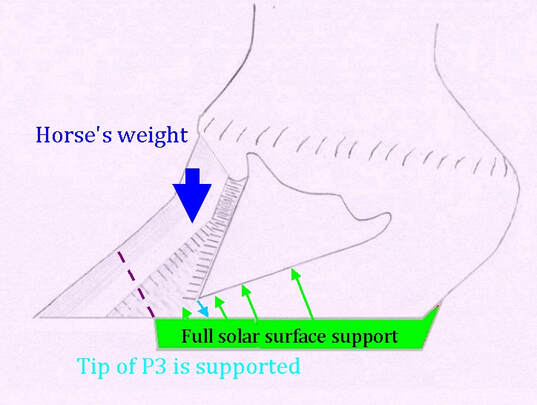
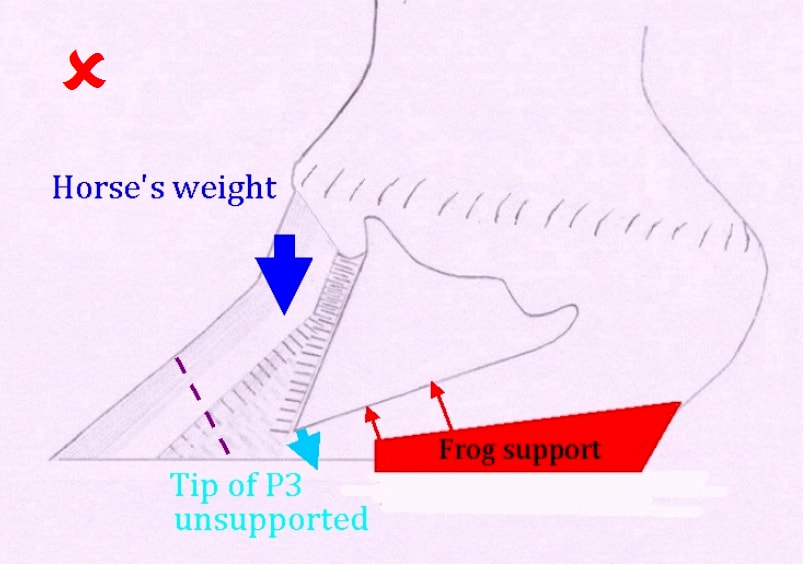
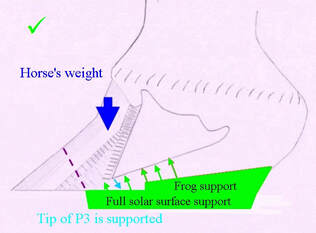
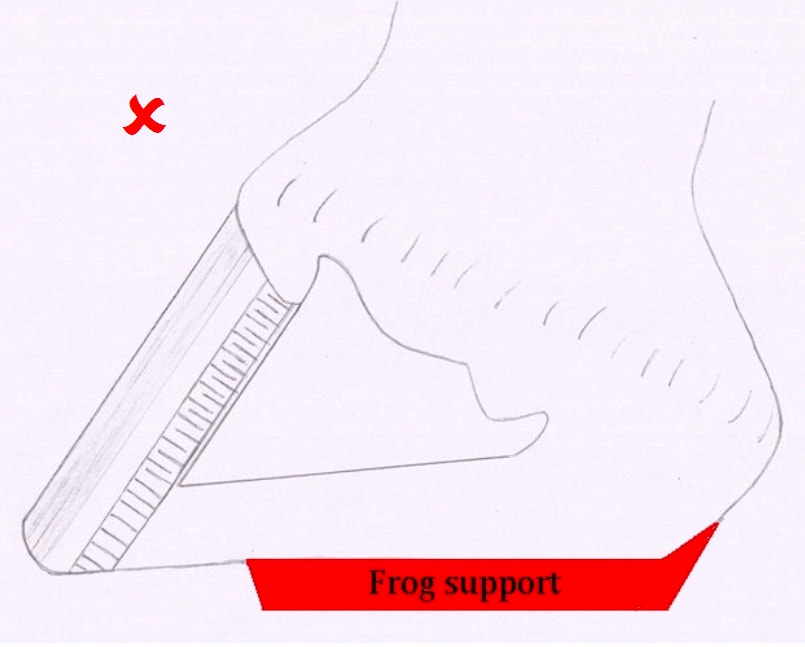
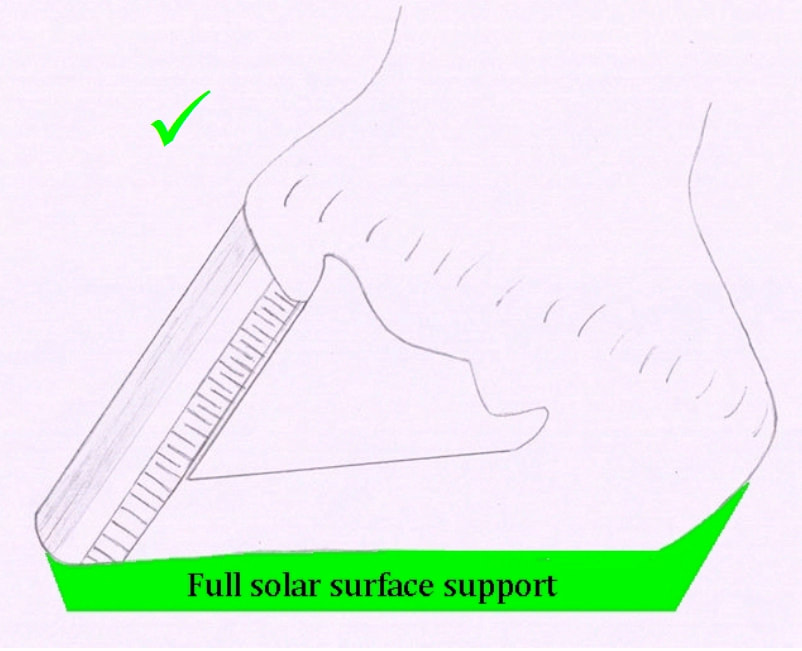
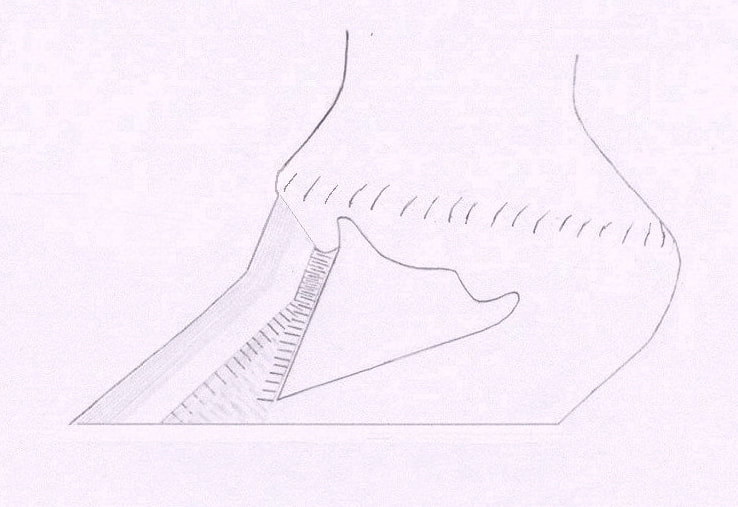
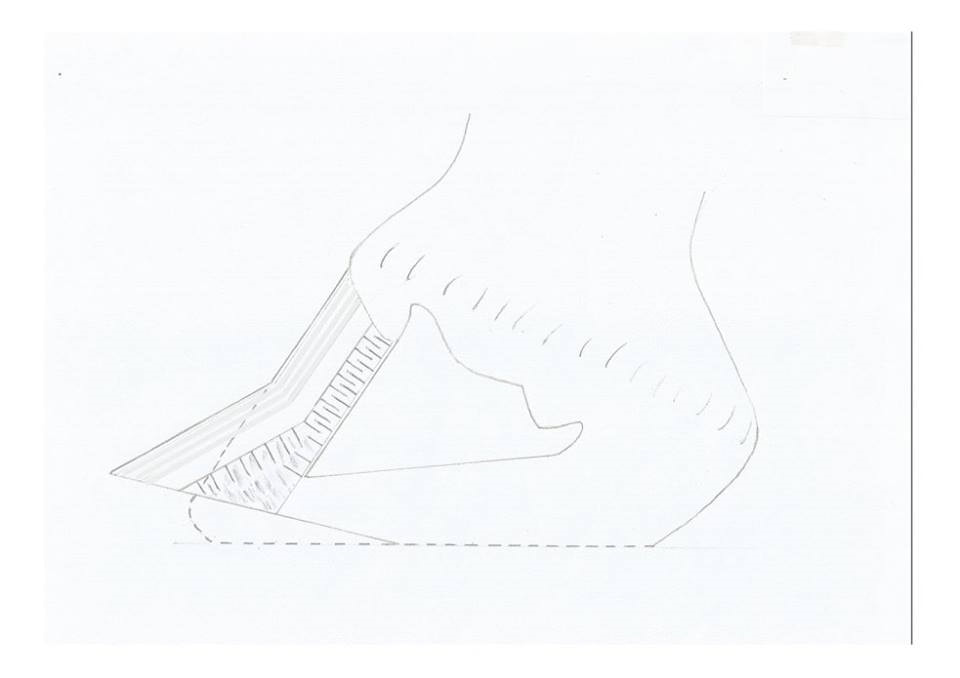
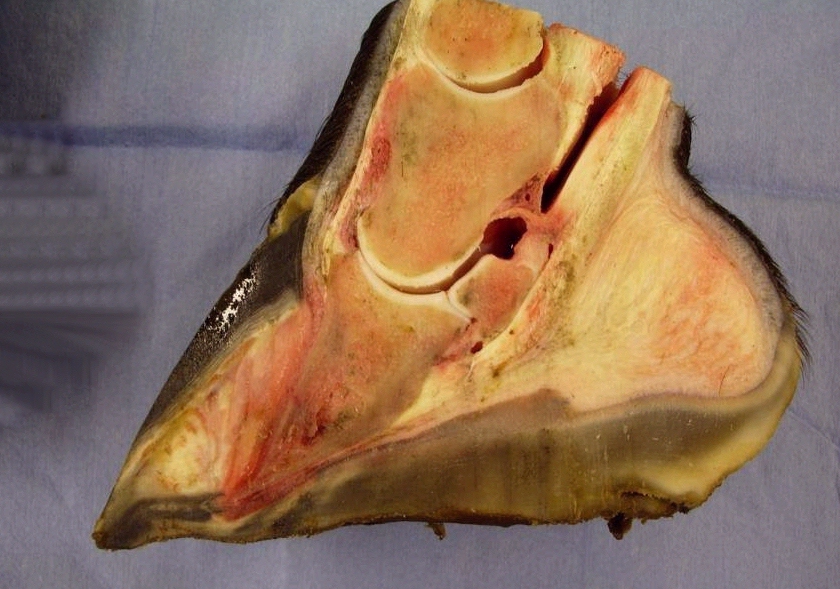
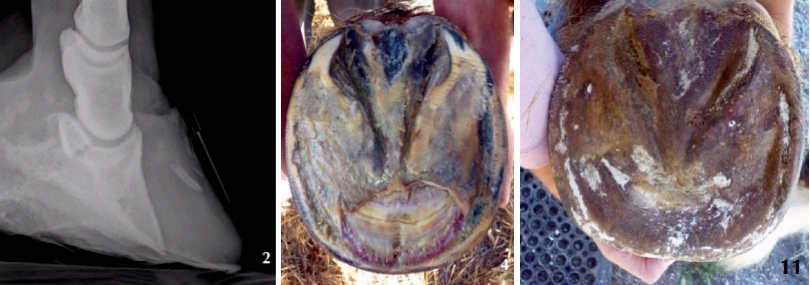
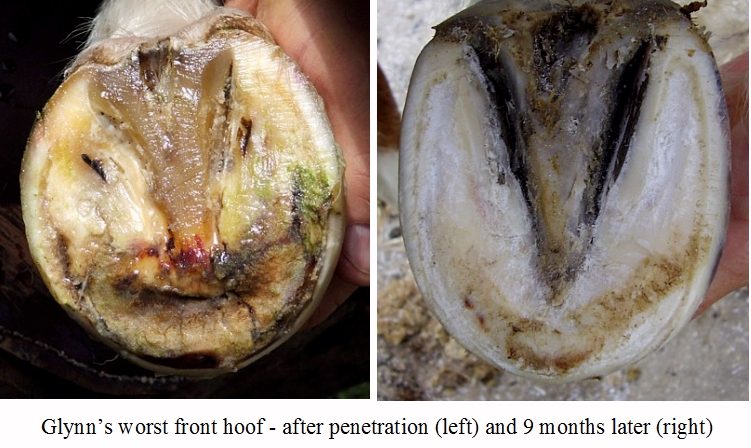
We will improve these graphics as soon as possible, but this article will hopefully help you to see a healthy non-laminitic foot (top) compared to a chronic laminitic foot (middle) or a laminitic foot that is showing risk factors associated with P3 penetration of the sole (bottom).















 RSS Feed
RSS Feed